
Most Southeast Asian nations were praised last year for their swift response to Covid-19, but now they're scrambling to curb a more infectious Delta variant that is surging across the world.
The challenge of dealing with the coronavirus has tested healthcare systems to their limits. But countries are also learning valuable lessons about new approaches and technologies, and how they can be applied to build more responsive and efficient healthcare systems for the future.
In Thailand, steps taken to keep the system from being overwhelmed, as well as to reduce the risk to frontline health workers, have included home isolation and hospitels, together with telemedicine.
But even when providers have the best of intentions, the system doesn't always work as well as it should for everyone who needs it, as Supamat Boonwattanasoontorn discovered.
Everyone in her family except for her father tested positive for Covid-19. "I called the 1330 hotline to register for home isolation and to find beds for my family members but after waiting for two days, I didn't get any callback," she told Asia Focus.
"A lot of people are being stranded. There is no point calling," said the 27-year-old account manager, who received one dose of AstraZeneca coronavirus vaccine in July.
Ms Supamat was in home isolation for five days, when an x-ray showed white patches in her lungs. "I was getting anxious, so I looked for a hospitel," she said.
Serving as a field hospital but with better facilities, a hospitel is a combination of hospital and hotel. Ms Supamat is now being treated in one in Pathum Thani.
But she has yet to meet the doctor supervising her care; she only hears his voice. "The doctor has telephoned to assess my symptoms every day. Medicines are distributed later according to the symptoms.
"Given the restricted situation, I think telemedicine is a good option."
Her routine in the hospitel includes regular checks of her blood oxygen levels and body temperature. "Being under the supervision of a doctor makes me feel much relieved as I don't know how to navigate the process," Ms Supamat admitted.
Sireethorn, a 25-year-old physician who started offering telemedicine services in late June, says she is getting used to the system.
She is now looking after patients with non-communicable diseases (NCD) such as Alzheimer's, diabetes and kidney disease, and Covid patients who are in home isolation.
For NCD patients, "I divided patients in half, for on-site check-ups and telemedicine," said Dr Sireethorn, who asked that her surname not be used.
Patients who have less complex medical conditions and adequate equipment at home, such as a glucose meter, will be offered telemedicine services. Those with worse conditions or with specific diseases such as Alzheimer's might need an on-site physical check-up.
Though Dr Sireethorn calls it an on-site check-up, it is not in person. "They will be in a room with a camera and microphone, talking to me in another room."
One challenge is that she needs to spend a lot more time taking a medical history in order to accurately diagnose patients since she can't physically examine them.
In Dr Sireethorn's opinion, telemedicine works well if she is familiar with a patient's case. It's more challenging for patients she doesn't know about, and this applies to Covid patients in home isolation.
Once someone is in home isolation, a hospital logistics team will send the equipment and medicine to the house including an oxygen meter, thermometer, cough medicine, and sometimes Favipiravir.
For new patients, she said, "I will have to explain how the treatment works. There will also be a little Q&A session: what kind of medicine they will get, will they get Favipiravir, and so on. This is so they know they are not being stranded.
"Then I will call them every day to check for fever and oxygen levels as well as any other symptoms."
It can be stressful, she admitted, especially with older patients who are not familiar with technology, as she uses the messaging app Line to connect with them.
"It's challenging from the start, just to accept a video call because sometimes I need them to take off their shirt so I could see the movement of the chest," she recalled.
Another time, she had to explain via video how to set up a home oxygen tank. "It was fortunate that he knew how to use Line."
"If telemedicine is here to stay, I think the issue is the access to video calling," Dr Sireethorn pointed out. Although a video call enables a doctor to perform an examination, not every patient has access to it, and not every phone or internet connection can produce a good quality video call.

DIGITISE NOW
The rise of technology and its potential for transforming service provision is one of the key factors influencing the change in the healthcare landscape in Asia Pacific, according to a report by Bain and Company.
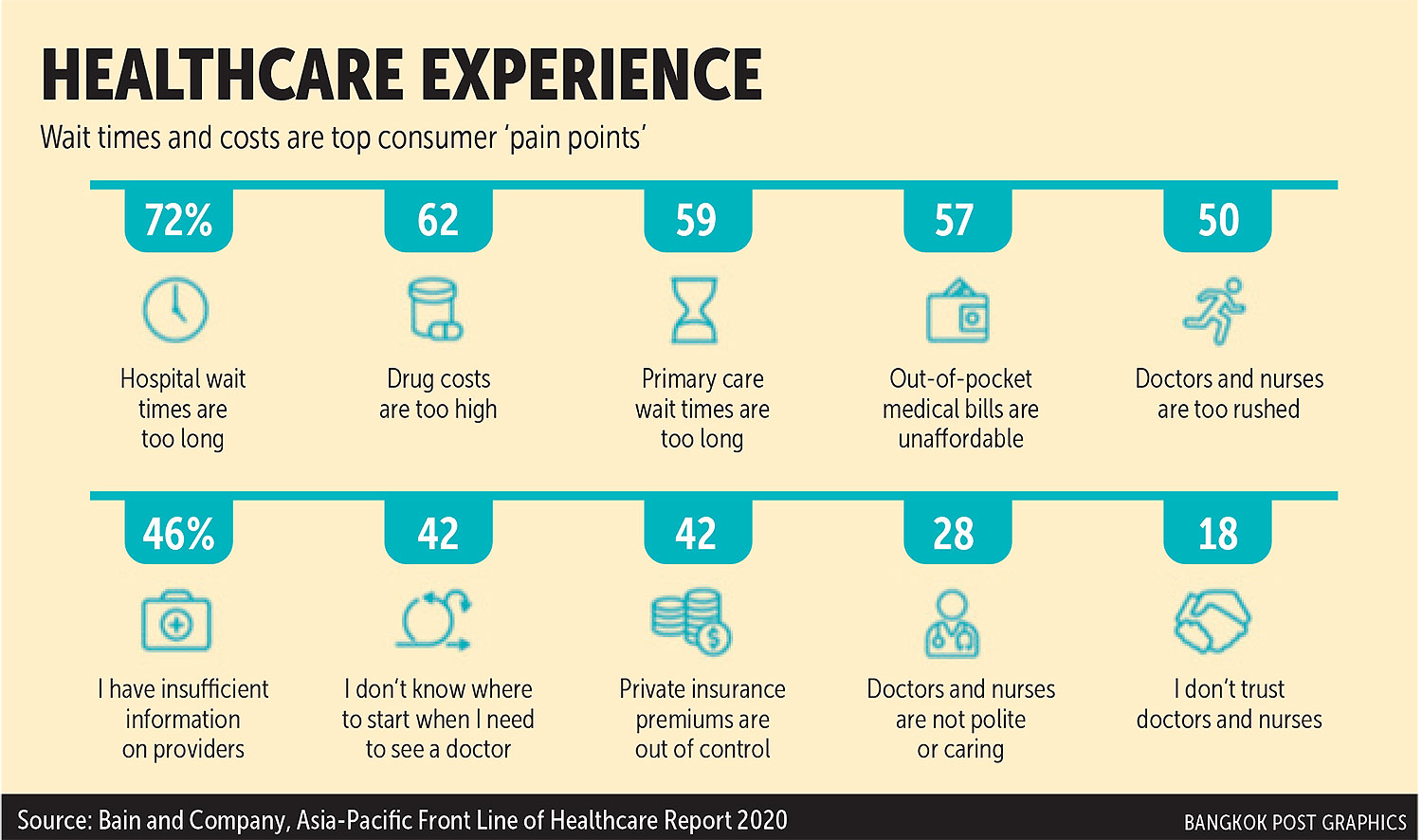
Bain surveyed 1,800 consumers in six regional markets -- Australia, China, India, Indonesia, Singapore and Thailand -- and also interviewed 250 physicians in Australia, China, India and Indonesia for the Asia-Pacific Front Line of Healthcare Report 2020.
First, the region's demographics are changing, with populations getting older and sicker. By 2025, 460 million people will be over 65 years of age.
At the same time, about 265 million will be diagnosed with diabetes. This will drive a shift from acute care services to chronic care management.
Rising costs are a concern across the surveyed countries. Fifty-seven percent of consumers said their out-of-pocket expenses for healthcare were unaffordable. Physician capacity is also a factor given the shortfalls in funding and resources, changing patient expectations, and cost barriers to new technology.
And despite Asia's enthusiastic embrace of the digital age, more needs to be done.
"The biggest gap that needs to be closed in Asia is the digitisation of the healthcare industry," said Sigal Atzmon, chief executive officer and founder of Medix, a London-based healthcare services provider.
No one was prepared for the pandemic. Most governments didn't prioritise digitisation. Instead, they focused on simply providing care, mainly through hospitals, and on the number of doctors, she said.
Ms Atzmon recommends that governments develop a comprehensive digital health records system and put it in the cloud so that both doctors and patients can access the information.

Not only will an information-heavy database help save lives, but it will also reduce the time needed to book medical appointments at hospitals.
"The development of these digital medical services will also help to significantly improve the accessibility and efficient deployment of doctors," she added.
In Israel, where medical records are fully digitised, the country had an immediate advantage when the pandemic first hit.
The government was in a position to immediately develop an app to communicate directly with people, and update their health records in real time. This included setting up a booking system for vaccines, and then following up on any side effects.
Healthcare policymakers all over Asia now realise "there is no option but to move forward and embrace the technological future of healthcare", said Ms Atzmon, who believes China has a head start.
"China started its digitisation a few years before the pandemic," she noted, adding that the country has an advantage in that all its medical records are in one language and centrally owned by the government.
The Chinese government has digitised both the central health system and systems in hospitals. Private companies are offered incentives to invest in the field.
WeDoctor, a Tencent-backed medical mobile app, provides a wide range of services from health treatment, insurance and online pharmacies to cloud-based software for hospitals. It aims to address key pain points in the sector: money, time and distance.
Patients can use the app to make medical appointments through 7,800 hospitals, both private and public, across China. It now hosts over 270,000 doctors and 222 million registered patients.
"The Chinese system works. I tried the app and you can easily book an appointment to see a doctor in most of China's cities," noted Ms Atzmon.
The app offers both Western and traditional Chinese diagnoses, both facilitated by artificial intelligence (AI). It also accepts payments from the public health insurance system that covers over 95% of the population.
Its competitor, the Alibaba-backed Ping An Good Doctor, provides similar services including telemedicine. In January 2020 when the coronavirus first emerged, the number of new users jumped nearly 900% from December 2019.
"Without the support of the government, this would never have been able to happen," said Ms Atzmon. "A lot of countries should look to China and learn from their process."

HEALTHCARE TRENDS
As digitisation gains further ground, we will see more innovations such as wearable devices that will play an important role in collecting vital patient data as well as facilitating medical record-keeping.
"For doctors, the technology allows them to diagnose and implement tailored treatments, which in turn will bring greater efficiency and affordability to the process," Ms Atzmon said.
The use of AI, medical information technology, telemedicine and home care services are all expected to increase, especially given what countries have learned from dealing with the pandemic.
When Covid was peaking in India, Medix created a telemedicine platform -- or rather a virtual hospital -- where patients could respond to live questionnaires about the severity and urgency of their symptoms. An algorithm then evaluates the severity of each patient's condition and the medical attention he or she will need.
If the patient has fallen ill or is showing obvious symptoms, the digital platform looks for ways to shorten waiting time and quickly confirm an appointment with a doctor or nurse.
Home care, meanwhile, is something no longer limited to the elderly, noted Ms Atzmon. Home-based monitoring and treatment of people with mild Covid symptoms has helped many countries, including Thailand, reduce the burden on hospitals.
"Home care is often more affordable, more accessible and is preferred by most people," she said, adding that it allows for a range of therapies to be provided at home, which helps speed up recovery from illness, injury or surgery. Family members can be a part of the rehabilitation process as well.
Machine learning, meanwhile, can make some hospital services more efficient. For example, patients normally have to wait for a doctor to review an MRI or CT scan, but machine learning will reduce the waiting time and assess the results. Only complex cases will need to be reviewed by doctors, giving them more time to see patients in greater need and thus alleviating physician shortages.
Another growing trend is personalised medicine, which Ms Atzmon said could lead to a "a revolution in cancer care and treatment".
"Personalised medicine uses information about your genetic background, or your disease or tumour, and applies this to tailoring treatments that best work for your condition," she explained. "Through our own genetics, we are finding out more about these life-threatening diseases and that is a game-changing development."
Just as everyone in the world has a unique genetic background, so "every medication in cancer care works differently for different people. Central to it all is genetics and the molecular analysis of every single cell, whether sick or healthy.
"As a result, each diagnosis requires a treatment that works specifically for that unique condition and person."
With more advanced technology, "I predict that we will make fewer trips to hospitals in the future. Everything will be online and remote through digital solutions," said Ms Atzmon, adding that healthcare "will be faster, less expensive and more accessible to many people".
Unlike other industries where technology can simply replace the workforce, the healthcare sector will still need high-level human expertise.
Ms Atzmon acknowledged that "machine learning is going to replace some parts of the medical system and, to an extent, elements of a doctor's day-to-day responsibilities", but "we will always need doctors. A doctor's role, particularly that crucial human interaction, is not replaceable".
Technology, in her view, will enhance doctors' skills and improve the decision-making process.

Sigal Atzmon, chief executive officer of Medix SUPPLIED
IMPROVING THE SYSTEM
Even before the pandemic, both physicians and patients in Asia Pacific were ready to embrace digital change. "Roughly 50% would adopt digital delivery models like telemedicine and remote care in the next five years," according to the Bain report.
"The need is greater now than ever before, and the pandemic has shown us that. The positive is that people have become far more receptive to innovation in healthcare," said Ms Atzmon.
"The acceptance comes from a real need. It's not a fad that will come and go. Telemedicine serves a real pain point and will close a worrying gap."
As governments do not have the resources to support an entire population's health needs, one route to ease the strain is to relax regulations and allow private companies to provide more services.
To accelerate the adoption of digitised healthcare, Ms Atzmon suggests governments focus on reducing bureaucratic procedures to attract investment. "They have to improve the regulation and adapt the law to the new healthcare landscape and urgent needs."
In many countries including Thailand, a lot of people pay out of pocket in order to have decent healthcare. "Governments, together with private insurance companies, must work together to create solutions for people so they have the protection to pay their medical bills," said Ms Atzmon.
"They need to introduce digital health solutions to ensure that healthcare is more accessible, quality-driven and affordable to all. The faster they set up a digital platform to help serve the people, the less expensive and more efficient the healthcare system will be. It's a win-win scenario."