In 2021, malaria caused 619,000 deaths, 77% of which were children under five, and 96% of them in Africa. But now, after decades of research -- and several false dawns -- a malaria vaccine known as R21/Matrix-M (henceforth just R21) has been shown to be effective in 70-78% of cases. Although three doses are required before that level of protection is reached, and a booster is needed one year later, the vaccine, developed at the University of Oxford and the Serum Institute of India, is cheap. It can be produced for US$2-$4 (70-140 baht) per dose -- comparable to the cost of other childhood vaccines.
Adding costs for delivery and administration, we can say that R21 costs approximately $5 per dose. A recent study indicates that fully vaccinating eligible children in areas where malaria is prevalent would save more than 600 lives per 100,000 children vaccinated, as well as prevent nearly 200,000 clinical cases of malaria. This suggests that the deaths of hundreds of thousands of children could be prevented for roughly $3,300 per life saved.
In October, R21 was recommended by the World Health Organization (WHO). It now needs to go through the WHO's prequalification process and receive the recommendation of the WHO's Strategic Advisory Group of Experts on Immunisation. Then a broad international rollout can begin.
Children eligible for R21 are between five months and three years old. About 80 million eligible children live in malaria-prone regions of Sub-Saharan Africa. To give them all three doses of the vaccine in 2024 would require 240 million doses, followed by a further 80 million boosters in 2025. After that, with the backlog of currently unvaccinated children dealt with, the roughly 30 million children born every year would need 120 million doses. This would save about 450,000 lives per year.
Saving a life for $3,300 is a bargain. In the US, Medicare covers the cost of kidney dialysis for patients over 65 who would otherwise die while awaiting a transplant. Fifteen years ago, economists from Stanford and Wharton calculated that the average cost per quality-adjusted year of life gained by this coverage was $129,000. Adjusting that figure for inflation (and overlooking the fact that medical costs have risen faster than other prices) takes it to $182,000 -- and that's just for one extra year of life. By comparison, if we conservatively estimate that the children saved by vaccination against malaria have a life expectancy of 50 years, the cost per year is $66.
Even when judged by global, rather than US, standards, saving a life for $3,300 is an exceptionally good value. The most cost-effective evidence-backed programmes that leading charity evaluator GiveWell has been able to find cost $3,500-$5,500 per life saved.
When vaccines for Covid-19 first became available, governments' highest priority was to get them through the regulatory process. The US Food and Drug Administration normally takes about ten months to authorise the use of a new vaccine, but it approved the use of the Pfizer vaccine in a breathtaking 21 days, and authorisation for Moderna's vaccine took just 19 days. WHO prequalification normally takes 270 days after the WHO recommends a vaccine. That is an unacceptable delay. The WHO should accelerate its process.
1Day Sooner was founded to represent people who wanted to volunteer to take part in human challenge trials to accelerate vaccine development. When the organisation was established in March 2020, its focus was a vaccine against Covid-19: getting it out one day sooner would save thousands of lives. Many of the organisation's staff and a high proportion of the volunteers were effective altruists.
The organisation's original mission has broadened to promoting efficient development of life-saving medical research and the speediest and most equitable distribution of its products. As part of that broader mission, 1Day Sooner set up 1Day Africa to promote vaccination on the continent by strengthening Africa's scientific capacity and its ability to manufacture vaccines locally.
Now, 1Day Africa is concerned that the WHO and national governments are not assessing the safety and effectiveness of the new malaria vaccine with the same urgency as they assessed the Covid-19 vaccines. As a result, the organisation is pressing for the production of as many doses of R21 as possible in 2024, and getting those doses into the arms of children as quickly as possible.
Some of the relevant facts are in dispute, including how long the WHO's prequalification process needs to take. But one thing should be clear: failing to save the lives of African children when that can be achieved for as little as $3,300 each would render hollow our lofty rhetoric about the equal worth of every human life. ©2023 Project Syndicate
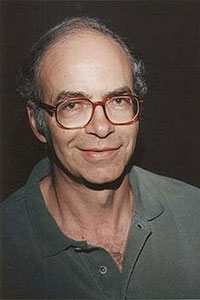
Peter Singer, Professor of Bioethics at Princeton University, is Founder of the organisation The Life You Can Save. He is the author of 'Practical Ethics, The Life You Can Save, Animal Liberation Now', and a co-author (with Shih Chao-Hwei) of the forthcoming 'The Buddhist and the Ethicist' (Shambhala Publications, December 2023).