We pull on layers to protect our vulnerable core. When they break, we are exposed and desperate for new shells, but they take time and do not come easily. Sometimes, we borrow them from the dead.
Skin is a natural barrier that shields the human body from external danger, including injury and germs. It sheds older cells and produces a new epidermis every month, but like other body parts, it is naturally susceptible to damage.
Medical advances redefine when life begins and ends. Kept in a small bottle in cold storage, the skin of a deceased donor can help burn victims, including those in the recent pub fire in Chon Buri, a doctor in charge of a local skin bank says, but the treatment remains unknown.
"Skin is retrieved from the dead and grafted onto burn victims in need of transplant," Dr Supanit Nivatvongs, deputy director of the Organ Donation Centre under the Thai Red Cross Society, said in an interview last week.

Dr Supanit Nivatvongs, deputy director of the Organ Donation Centre under the Thai Red Cross Society. The Organ Donation Centre
"Normally, patients can supply skin from other parts of their bodies [autograft], but in case of severe damage, cadaver skin can come in handy like bandage [allograft]. Biological dressing can prevent loss of water, protein, minerals and heat. It can also reduce contamination and pain."
There are three levels of burns, based on the severity of damage. Victims suffering second- and third-degree burns should receive skin transplant, he said.
Eighty percent of burn victims who have over half of their bodies destroyed are likely to die, according to the centre.
Dr Supanit said there are many treatment options. While autograft skin will stay on, allograft will peel off in two weeks, after "allowing time for new skin to grow". In case of deep wounds, autograft is still required, but patients will already pass the critical period. Lastly, artificial skin works on the same principle, but requires regular change and costs a lot.
"Allograft will come off naturally. Patients don't have to clean the wounds often, reducing pain and expense," he said.
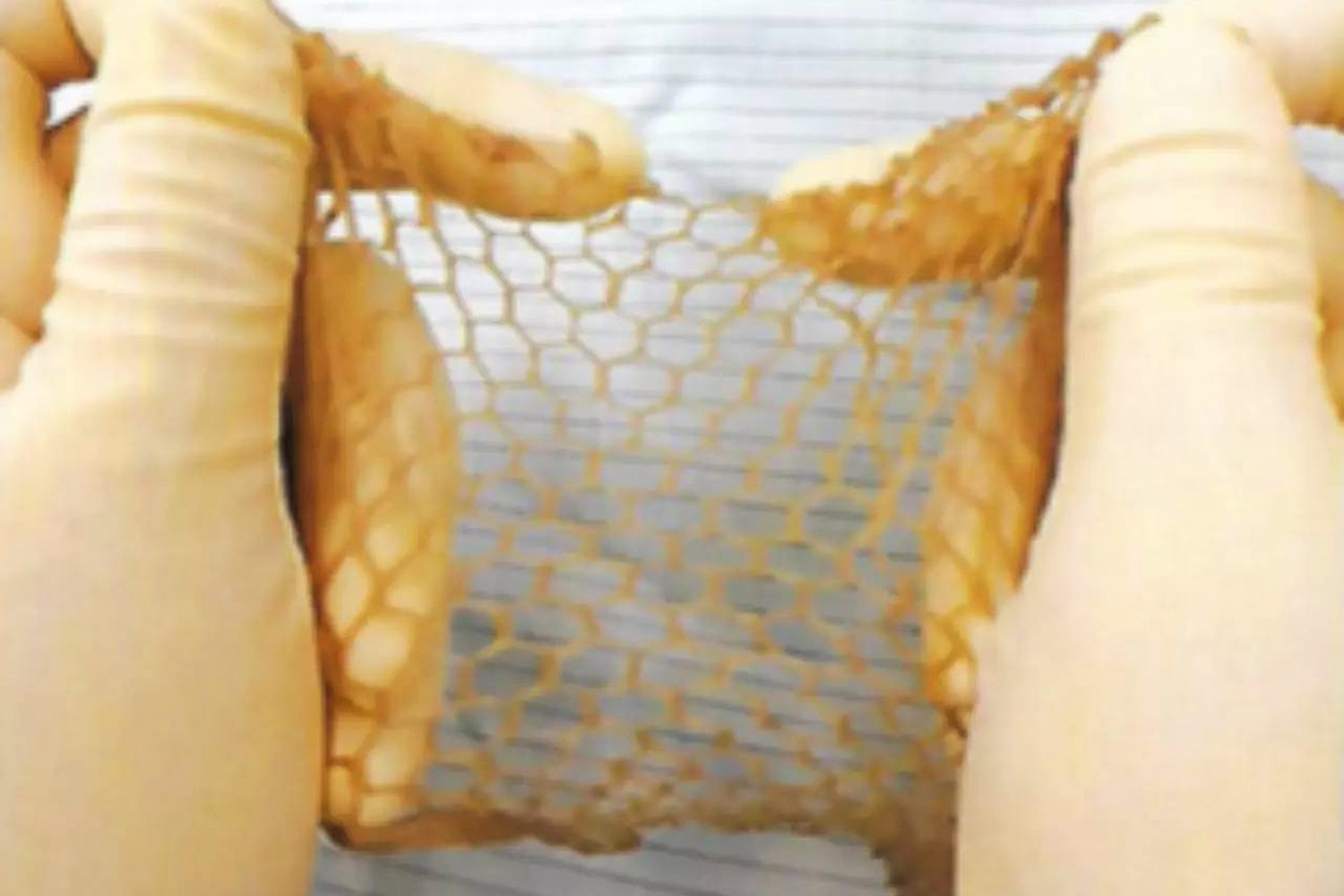
Skin retrieval takes around a week. First, staff screen deceased donors for infectious diseases, wounds and tattoos, regardless of the cause of death. After removing skin using dermatome, they clean and process it several times. Finally, they place prepared skin in a special liquid -- glycerol -- at a temperature of 4C.

Staff prepares human skin.
"We collect skin from backs and thighs because they are larger and more useful than other parts," he said. "It is put in a plastic bottle and labelled with details, including production date, size and expiry. Theoretically, it can be kept for five years, but should be used in two years."
Skin removal should be conducted in a timely manner, about six hours if the deceased donor dies at room temperature or 12 hours in a cold room, he said.
While donors can die of any cause, most of them suffer from brain death (65%) and circulatory death (35%). The annual average of skin donation is around 100,000cm², but in the aftermath of the coronavirus pandemic, it has fallen to around 60,000cm².
"In the case of the Mountain B pub fire, we have used nearly 30,000cm². A fatal accident typically expends a lot of resources," he said.
Challenges include lack of staff and network. Founded in 2015, the skin bank has struggled with its manpower. A small team of trained staff must collect skin from hospitals themselves. When the outbreak hit, they were not allowed to work on the ground, but the situation is getting better.
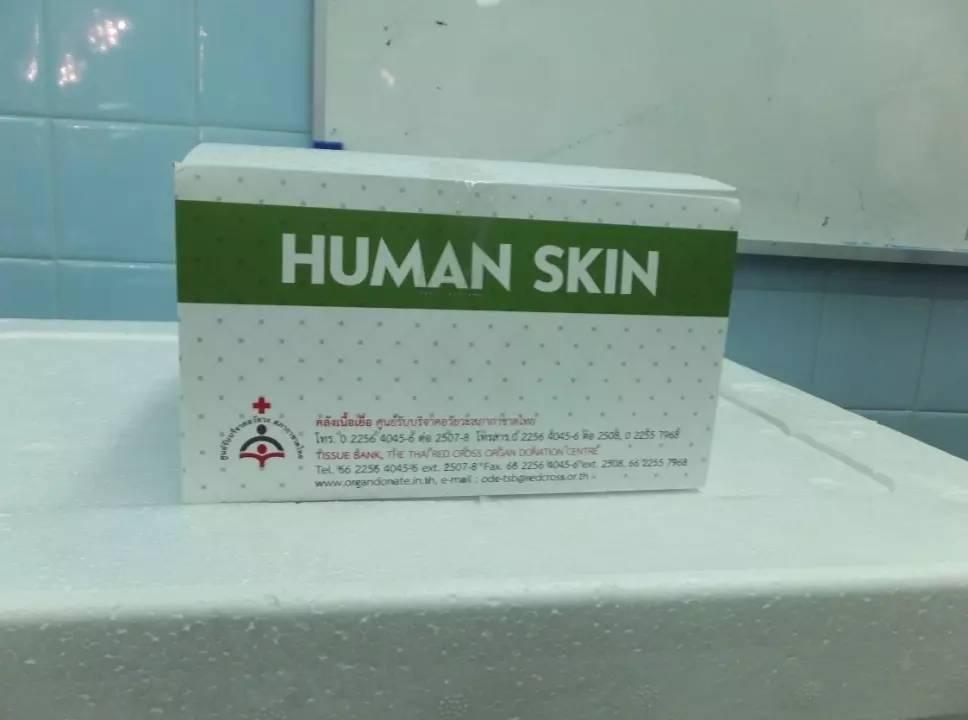
The skin of deceased donors can help burn victims.
"Currently, we have around 30,000cm², but it should have hundreds of thousands in store for emergencies. We are trying our best to increase supply," he said.
The skin bank is the only source of donated skin. In fact, hospitals can retrieve tissues from donors, but they do not have skin transplant facilities.
Dr Supanit noted "some doctors are unfamiliar with the technique" of cadaver skin transplant. It has been discussed in academic conferences for years, but they are reluctant to carry out the procedure.
Dr Supanit said allograft is not covered by any health schemes. The skin bank is launching a campaign for free transplant until the end of September. It has drafted a plan to continue the service for five years, pending the government's approval, to provide an option for doctors and patients.
"Artificial skin is imported from foreign countries. It yields similar results to human skin, but costs a lot and entails economic loss," he said.
A wave of fires necessitates a large supply of donated skin. Early this month, flames engulfed the Mountain B pub in Chon Buri, reminiscent of the Santika pub fire in Bangkok over a decade ago. Last week, insurgents launched co-ordinated bomb and arson attacks on convenience stores and petrol stations in three southern border provinces, causing injuries.
"While minor fires go unnoticed, high-profile cases, for example the southern unrest and gas explosions, recur. We must be prepared for them," he added.
The anatomy of the skin
Skin is the largest and fastest-growing organ in the body. It consists of three layers: the epidermis (outer), the dermis (middle), and the subcutaneous tissue (deep). Each contains specific cells, vessels, glands and receptors. It gives protection, regulates body temperature, works as a sensory organ and produces vitamin D.
Guidelines for skin donation
- No minimum age up to 80
- Weigh at least 50kg, minimum height 150cm
- Free of diseases, including hepatitis, HIV/Aids, syphilis, cancer
- Free of wounds, scars, skin diseases, tattoos, etc
- Free of drug use and criminal history within a year before death
For more information, contact the skin bank at 1666, 02-256-4045/6 ext 2508, 092-247-9864 or add Line ID: odctsb.